- India
- International
Explained: Amid coronavirus outbreak, a look at epidemics that have hit India since 1900
The World Health Organization defines epidemics as “the occurrence in a community or region of cases of an illness, specific health-related behaviour, or other health-related events clearly in excess of normal expectancy.
 Among other causes, mass travel has contributed to the rapid and more frequent spread of viruses around the world in an unprecedented way. (AP Photo)
Among other causes, mass travel has contributed to the rapid and more frequent spread of viruses around the world in an unprecedented way. (AP Photo)
Although India may have witnessed widespread illnesses and virus outbreaks in parts of the country, including the SARS outbreak between 2002-2004, statistics show that since the 1990s, they were nowhere as widespread as the COVID-19, that has now reached almost every part of the country and almost every country in the world. Among other causes, mass travel has contributed to the rapid and more frequent spread of viruses around the world in an unprecedented way.
What is an epidemic?
The World Health Organization defines epidemics as “the occurrence in a community or region of cases of an illness, specific health-related behaviour, or other health-related events clearly in excess of normal expectancy. The community or region and the period in which the cases occur are specified precisely. The number of cases indicating the presence of an epidemic varies according to the agent, size, and type of population exposed, previous experience or lack of exposure to the disease, and time and place of occurrence.” Epidemics are characterised by the rapid spread of the specific disease across a large number of people within a short period of time.
 A Telangana State Road Transport Corporation (TSRTC) worker disinfects a bus as a precaution against COVID-19 in Hyderabad, (AP Photo/Mahesh Kumar A.)
A Telangana State Road Transport Corporation (TSRTC) worker disinfects a bus as a precaution against COVID-19 in Hyderabad, (AP Photo/Mahesh Kumar A.)
Many Indian citizens born at the start of the 21st century have not fully witnessed or experienced circumstances surrounding the mass outbreak of epidemics in the country and for many, the challenges brought by the rapid spread of COVID-19 is unknown territory. This is not to say however, that as a nation, India is completely unfamiliar with dealing with epidemics and public health crises, some with exceptional success. indianexpress.com tracks epidemics that have occurred in the country since the 1900s.
📢 Express Explained is now on Telegram. Click here to join our channel (@ieexplained) and stay updated with the latest
1915-1926 — Encephalitis lethargica
Encephalitis lethargica, also known as ‘lethargic encephalitis’ was a type of epidemic encephalitis that spread around the world between 1915 and 1926. The disease was characterised by increasing languor, apathy, drowsiness and lethargy and by 1919, had spread across Europe, the US, Canada, Central America and India. It was also called encephalitis A and Economo encephalitis or disease.

According to Dr. J.E. Dhunjibhoy, an Indian doctor who conducted research on the disease and published his findings in July 1929, the virus was then considered to be an “acute contagious disease” where the virus “attacks the central nervous system…and grey matter”. The research goes on to say that it spread across Europe in 1917 after having first been discovered in Vienna in the same year. However, despite being witnessed in an epidemic form in Europe between 1917-1929, it was still “sporadic” in India by 1929. This virus, according to Dr. Dhunjeebhoy’s notes, appeared to be spread through nasal and oral secretions. Approximately 1.5 million people are believed to have died due to this disease.
1918-1920 — Spanish flu
Before most of the world had recovered from the spread of Encephalitis lethargica, there was a new virus to contend with, the Spanish flu. This epidemic was a viral infectious disease caused due to a deadly strain of avian influenza. The spread of this virus was largely due to World War I that despite drawing to a close by the time the epidemic had peaked, has caused mass mobilisation of troops in various parts of the world, whose travels helped spread this infectious disease. There are contradicting reports concerning the total number of fatalities caused by this disease around the world, but researchers say that the death toll was significantly more than 50 million people. In India, approximately 10-20 million people died due to the Spanish flu, that was brought to the region a century ago, by Indian soldiers who were part of the war. During this pandemic, however, records show that word spread of the dangers of the disease, through official government channels as well as word of mouth. People began taking basic precautions of engaging in forms of social distancing and limited travel, perhaps contributing to the disease eventually tapering off in India.
1961–1975 — Cholera pandemic
Vibrio cholerae, one type of bacterium, has caused seven cholera pandemics since 1817. In 1961, the El Tor strain of the Vibrio cholerae bacterium caused the seventh cholera pandemic when it was identified as having emerged in Makassar, Indonesia. In a span of less than five years, the virus spread to other parts of Southeast Asia and South Asia, having reached Bangladesh in 1963 and India in 1964. In India, researchers have observed in academic papers that Kolkata’s climate and location in the Gangetic delta, including poor practises in water sanitation, make the city a hotbed for cholera and this pandemic was no different.
From South Asia, it spread to the Middle East, North Africa and then onwards to Europe. In this case as well, decreasing levels of sanitation, increasing populations and increased international travel contributed to the spread of bacteria across the world. By the 1970s, the bacteria had spread to Japan and the South Pacific. Medical research suggests that by 1991, it had spread to Latin America, where it killed approximately 10,000 people in Peru alone. By that time, the number of reported cases around the world totalled 5,70,000.
1968-1969 — Flu pandemic
This flu pandemic was caused by the H3N2 strain of the influenza A virus and appears to have emerged in Hong Kong in July 1968. It did not take much time for the virus to spread around the world. Soon after the discovery of the presence of the virus in Hong Kong, by the end of July 1968, the outbreak spread to Vietnam and Singapore. In two months, it had spread to the Philippines, India, Australia and parts of Europe.
American soldiers returning from Vietnam after the Vietnam War in September 1968, brought this virus to the US, with the first few cases having been detected in California. By December that year, the virus had become widespread across the US. In 1969, the virus spread to other parts of the world, including Japan, Africa, South America. In the span of one year, the virus was estimated to have killed approximately 1 million people around the world.
1974 — Smallpox epidemic
According to WHO, smallpox was officially eradicated in 1980. The infectious disease was caused by either of the two virus variants Variola major and Variola minor. Although the origins of the disease are unknown, it appears to have existed in the 3rd century BCE. This disease has a history of occurring in outbreaks around the world and it is not clear when it was first observed in India. By 1950, the World Health Organization had begun laying plans for mass-eradication campaign of smallpox around the world, and despite the costs and ambitious plans, global support for this campaign had increased.
According to the University of Michigan, in the early 1960s, 60% of all smallpox cases in the world were reported in India, and this strain of the virus appeared to be more virulent than that found in West Africa. Given the concerning situation, India launched the National Smallpox Eradication Program (NSEP) in 1962 with plans to engage in mass vaccination of the population to curb the disease. The program did not bear the desired results, in part to the size of the population and socio-cultural and demographic challenges.
By 1966, although the disease had been eradicated in approximately 22 countries, it was still endemic in several other developing nations including in the Indian subcontinent, Indonesia and Brazil. This disease resulted in the death of millions of people around the world in the 20th century alone, and countless more since it was first recorded.
Between 1972-1975, the WHO along with medical assistance provided by the Soviet Union, specifically its supply of millions of doses of freeze-dried smallpox vaccine to India, helped administer the smallpox vaccine across the country and independent investigations revealed that India was free of smallpox by March 1977.
1994 — Plague in Surat
In September 1994, pneumonic plague hit Surat, causing people to flee the city in large numbers. Rumours and misinformation led to people hoarding essential supplies and widespread panic. This mass migration contributed to the spread of the disease to other parts of the country. Within weeks, reports emerged of at least 1,000 cases of patients afflicted with the disease and 50 deaths.
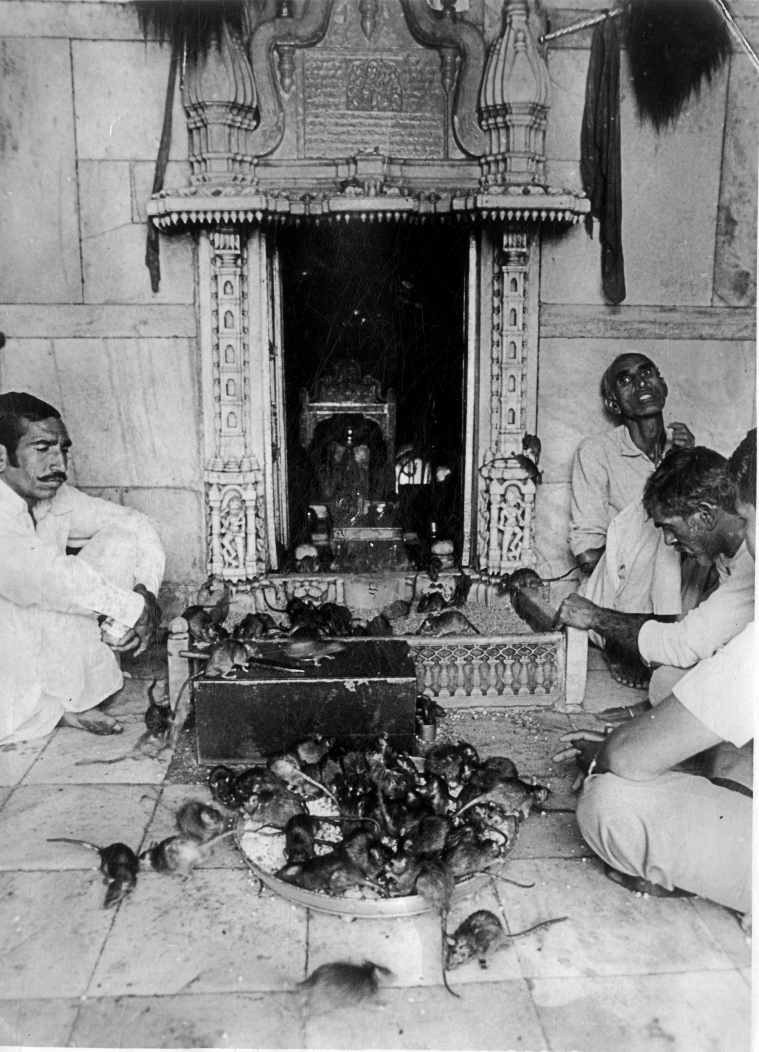 Despite the plague stalking the neighbouring Gujarat state, there is no dearth of people who worship rats at the famed Deshnouk Shrine in Rajasthan. Express archive photo
Despite the plague stalking the neighbouring Gujarat state, there is no dearth of people who worship rats at the famed Deshnouk Shrine in Rajasthan. Express archive photo
Open drains, unsanitary garbage disposal, unclean distribution of piped water, dead rats lying in the open drains, all collectively contributed to the plague outbreak in a city that had not been built for the migrant population living within its growing confines. Following the outbreak, the local Surat government was jolted into clearing up garbage and closing drains and managed to control the situation within weeks. However, the mismanagement of the city went back to the way it was soon after.
2002-2004 — SARS
SARS was the first severe and readily transmissible new disease to have emerged in the 21st century. In April 2003, India recorded its first case of SARS, severe acute respiratory syndrome, that was traced to Foshan, China. The patient was a man who was believed to have contracted the disease in Singapore. Similar to COVID-19, the causative agent of SARS was a type of coronavirus, named SARS CoV, that was known for its frequent mutations and spread through close person-to-person contact and through coughing and sneezing by infected people. In the two years, in total three cases of SARS were recorded in India. The virus had managed to spread to at least 30 countries around the world.
 Across the country, at least 50 people died in 2006 due to dengue. (Express photo: Praveen Khanna)
Across the country, at least 50 people died in 2006 due to dengue. (Express photo: Praveen Khanna)
2006 — Dengue and chikungunya outbreak
Several states in India reported simultaneous outbreaks of dengue and chikungunya virus in 2006 that affected people in several states across the country, including the Andaman and Nicobar Islands. Both are mosquito-borne tropical diseases and stagnation of water provides breeding ground for these mosquitoes that impact local communities. The chikungunya outbreak impacted Tamil Nadu, Andhra Pradesh, Karnataka, Maharashtra and several other states in the country. That same year, New Delhi and the states of Rajasthan, Chandigarh, Uttar Pradesh, West Bengal and Andhra Pradesh reported spikes in the number of patients with dengue, with the highest number of patients in Delhi. Across the country, at least 50 people died that year due to dengue.
 A municipal worker fumigates a residential area to check the spread of mosquito-borne diseases in New Delhi. (AP Photo/Manish Swarup)
A municipal worker fumigates a residential area to check the spread of mosquito-borne diseases in New Delhi. (AP Photo/Manish Swarup)
2009 — Gujarat hepatitis outbreak
In February 2009, reports emerged that approximately 125 people in Modasa, Gujarat, were infected with hepatitis B, an infectious disease caused by the hepatitis B virus that affects the liver. The disease is caused due to transmission of infected blood and other body fluids and local doctors were suspected of having administered treatments on patients with used and contaminated syringes. The Gujarat state government set up public initiatives to increase awareness of the disease as well as mass immunization under state medical authorities.
2014-2015 — Odisha jaundice outbreak
Several towns in Odisha witnessed an outbreak of jaundice in September 2014, with the first few cases having been reported from the town of Sambalpur. Within three months, at least six people had died and more than 670 cases of jaundice had been reported in the town. Investigators concluded that drain water had possibly seeped through pipe lines for drinking water, contaminating hundreds of people. By February 2015, the contamination of water had reached neighbouring towns and districts like Jajpur, Khorda and Cuttack and at least 3,966 cases of jaundice had been reported from across the state. The official death toll according to the Odisha state government was 36 but researchers estimated it to be higher, closer to 50.
 By March 2015, according to India’s Health Ministry, approximately 33,000 cases had been reported across the country and 2,000 people had died due to swine flu. (Express photo: Praveen Khanna)
By March 2015, according to India’s Health Ministry, approximately 33,000 cases had been reported across the country and 2,000 people had died due to swine flu. (Express photo: Praveen Khanna)
2014-2015 — Swine flu outbreak
In the last few months of 2014, reports emerged of the outbreak of the H1N1 virus, one type of influenza virus, with states like Gujarat, Rajasthan, Delhi, Maharashtra and Telangana being the worst affected. By February 2015, India reported at least 12,963 affected cases and 31 deaths. The virus spread to other parts of the country, prompting the Indian government to initiate public awareness drives. By March 2015, according to India’s Health Ministry, approximately 33,000 cases had been reported across the country and 2,000 people had died.
2017— Encephalitis outbreak
Although the city of Gorakhpur in Uttar Pradesh has had a history of being affected by encephalitis, in 2017, it witnessed an increase in numbers where several children died of encephalitis, specifically Japanese encephalitis (JE) and acute encephalitis syndrome (AES), caused primarily due to mosquito bites. Both are viral infections that cause inflammation of the brain leaving long-term physical disabilities and even resulting in death.
 The precise cause of AES which killed more than 350 in Bihar in 2014, is not known though a majority of medical professionals say it is linked to a heat wave that had gripped Bihar. (Photo by Ritesh Shukla )
The precise cause of AES which killed more than 350 in Bihar in 2014, is not known though a majority of medical professionals say it is linked to a heat wave that had gripped Bihar. (Photo by Ritesh Shukla )
The outbreak in Gorakhpur was attributed to the lack of cleanliness and sanitation in certain districts that had become breeding grounds for mosquitoes. Further compounding the problem, in a state-run hospital in the city where many children were being treated, oxygen supplies were cut off by the supplier due to non-payment of dues, leading to the deaths of several children. By September 2017, more than 1,300 children had died.
2018 — Nipah virus outbreak
In May 2018, a viral infection attributed to fruit bats was traced in the state of Kerala, caused by the Nipah virus that had caused illness and deaths. Within days of medical practitioners confirming the outbreak of the virus, the Kerala government stepped in to implement several protectionary measures to contain the spread of the virus and to initiate information sharing drives with the public.
 Health officials remove waste from an isolation ward of Ernakulam Medical College in Kochi. (PTI)
Health officials remove waste from an isolation ward of Ernakulam Medical College in Kochi. (PTI)
The spread of the outbreak remained largely within the state of Kerala, due to efforts by the local government and various community leaders who worked in collaboration to prevent its spread even inside the state. These measures included issuing travel advisories, the establishment of medical facilities and the suspension of large public gatherings, including religious congregations. Between May and June 2018, at least 17 people died of Nipah virus and by June, the outbreak was declared to have been completely contained.
More Explained
EXPRESS OPINION
Apr 26: Latest News
- 01
- 02
- 03
- 04
- 05