- India
- International
K Srinath Reddy: ‘We have to wait for two more weeks to see if the curve has flattened’
Coronavirus (COVID-19): "In this large country, we will need state wise or preferably even district wise assessments, as the calendar of the epidemic and its control will vary across the country. I will look at the number of new cases per day as a fraction of the number of lab and clinical assessments performed that day, using comparable criteria for case definition," said Professor K Srinath Reddy.
 “The rise in numbers have to be interpreted in the context of the number of type of tests performed at different periods,” said Professor K Srinath Reddy. (Express photo by Prashant Nadkar)
“The rise in numbers have to be interpreted in the context of the number of type of tests performed at different periods,” said Professor K Srinath Reddy. (Express photo by Prashant Nadkar)
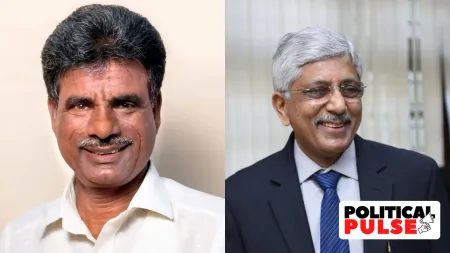
Coronavirus (COVID-19): Professor K Srinath Reddy, president of Public Health Foundation of India and a member of the high-level committee of public health experts for COVID-19 speaks to Kaunain Sheriff M on the fight against the pandemic. Excerpts:
On March 30, India reported 1251 COVID19 cases and 32 deaths; in less than a week, the country has witnessed an over 200 percent spike (4,000 positive cases and 109 deaths). Keeping two factors in mind, the lockdown that began on March 25 and at least 1495 cases linked to the Tablighi Jamaat congregation in Delhi, has India’s COVID curve peaked? What are the key dates and statistics that you are looking at, that will be critical in determining if India has been able to contain the spread of pandemic after the lockdown?
The rise in numbers have to be interpreted in the context of the number of type of tests performed at different periods. They have to be comparable during the two periods. We have to wait for two weeks more to see if the rising curve has flattened or is moving down. In this large country, we will need state wise or preferably even district wise assessments, as the calendar of the epidemic and its control will vary across the country. I will look at the number of new cases per day as a fraction of the number of lab and clinical assessments performed that day, using comparable criteria for case definition. I will also look at the number of serious acute respiratory infection cases hospitalised each day. I will seek supportive information from lab based random sample surveys and household syndromic surveillance data from both rural and urban samples. The immediate impact of the lockdown can be gauged over the next two weeks but the effort to quell the epidemic has to go on longer. It is only by June that we will get a measure of our success or continuing challenge. We need to do regular assessments against the backdrop of a progressive stepwise relaxation of the lockdown.
Virologists are very clear that it is the virus that determines the timeline, not us. However, most of the discourse around the pandemic is how long is the long haul? What is your view? What is the indicator, either at the centre or disaggregated at the states, to say that it is no longer a public health emergency? Is that a hotspot at Mumbai or Delhi, the number of new cases every day starts falling? What is the indicator?
The virus cannot be left to determine the timeline at its own pace. We have to do our best to slow down and then interrupt the transmission so that the virus fades out. Though the alternative of herd protection through 60% getting infected sounds attractive, that comes at a high cost of lives if the health system is not prepared for an early surge of serious cases. The signals that we are gaining control over the virus will come when the numbers of new cases, identified through a combination of testing and clinical criteria, consistently fall over 14 days. These data have to be disaggregated for each district and supported by random sampling survey in the district. Policy related to hotspots will also be driven by this, though the case rate fall may need to be consistent over a longer period of four weeks.

 K Srinath Reddy, president of Public Health Foundation of India.
K Srinath Reddy, president of Public Health Foundation of India.Over 80% of the total positive cases have been traced to 62 districts; and out of the 700 districts, more than 500 districts are almost Corona free. How do we keep increasing these numbers? And in your view what has the lockdown achieved?
The lockdown has achieved the slowing down of viral transmission, even it may not have fully stopped it. It has given time to prepare the health and social systems time to prepare for the delivery of essential services as the lockdown is progressively relaxed.
Also Read | Investors unfazed by March mayhem, equity MF inflow at 12-month high
It has achieved a high level of social solidarity that is needed to meet the national health emergency. It has brought central and state governments of different political parties together to work together with the common purpose of overcoming this massive threat. We have also identified good models from different states and districts where control measures were effective, for adoption and scale up elsewhere. If we work to plan, absorbing global and national learnings, but adapting to local conditions and trends to make data driven decisions, we can move all districts to the corona free category.
A common discourse around the pandemic is that the World is flat. For instance, when the US or UK is arguing for more PPE, India is also doing the same. As one of India’s biggest public health expert, what do think of the common discourse? How important is the public in public health?
I believe that even when the advocates of economic globalisation enthusiastically advocated the idea of the world becoming flat, the flat surface was tilted in favour of the advanced economies. The moment developing economies started exhibiting their economic muscle, protectionism surfaced in the rich countries. Even in the pandemic, the scramble for PPEs and ventilators is leaving the developing nations behind. Mr Trump’s threat that he will punish India if we do not export hydroxy-chloroquine was a blatant power play, not a polite request. Self reliance, even in the era of economic globalisation, has to be the new economic reality.
Also Read | Higher spend, slump in revenues start straining finances of states
However, the pandemic does highlight the shared vulnerability of humanity to microbes which do not recognise political borders drawn by humans. We have to move beyond that recognition to shared values which will bind humanity together and promote global health. Pandemic preparedness, anti-microbial resistance, re-engineering of our food and agricultural systems for improving health and nutrition, combating climate change and creating addiction free and non-violent societies are areas where shared values must erect the new edifice of global health. The public becomes the key transformational agent for such change. We must also freely share knowledge, without commercially motivated proprietary barriers. As Portuguese writer Miguel Targo observed, ‘ universal is local, without the walls’.
At least 7 states have indicated that they would continue to have restrictions in place even after the 21-day national lockdown ends. If you have to advice the government on what should be the next step, what would it be? What are the metrics you are looking at?
We have to find a path that helps us meet our priorities of public health protection, economic stability and social development. Foremost priority now is to prevent the epidemic from claiming many lives. At the same time we need to ensure that the economy does not grind to a halt, especially in farming and production of essential goods. Schools and colleges cannot remain closed indefinitely.So, we need to release the country from lockdown in a measured stepwise manner, balancing these priorities. Hot zones should be sealed off but strongly supported, warm zones should have intense surveillance and unaffected zones should start functioning near normally under watch. Older persons and persons with health conditions which increase vulnerability should continue to avoid exposure and greatly limit out-of-home movement. Travel should be permitted but prioritised for essential needs. Schools should reopen first and then colleges. Mass gatherings of any kind should be prohibited for a year. Monitoring of the epidemic will require data from random population sampling of every district with lab tests, household visits for syndromic surveillance by frontline health teams supported by community volunteers and backed up by medical teams, and hospital data on severe acute respiratory infections and deaths.
You have been invited by the WHO to be a member of the Executive Group of the steering committee of COVID19. Recently, Anthony Fauci shared a conversation he had with his counterparts at the weekly WHO meeting. He said that “some of the most cogent concerns” was that experts need to “keep an eye on balance” about the “unintended consequence” triggered by the lockdown and that such disruption can “result in poverty and other health issues unrelated to the coronavirus”. Don’t you think that a long lockdown, particularly in India with significant comorbidities, can drastically interrupt access to public health, especially the tertiary care? What is your view on the unintended consequences on poverty and health?
I am on the Executive Group of the Steering Committee of SOLIDARITY, a multi-country trial testing the efficacy of different treatments for COVID19. I am an independent technical expert and have no influence on WHO policy. I do agree that our battle against this pandemic should not lead to neglect of other health system functions, at all levels of care.
Don’t miss from Explained: Armed forces in outbreak battle: their role, procedures for requisition
Even for this pandemic, primary care is vital and we should not focus only on tertiary care. Social protection programmes too must not be derailed, especially at a time of economic disruption. A mature policy response will find the right balance, even though the immediate threat is what captures the attention. The lockdown cannot be protracted but must be timed to the right extent to effectively push back the threat that is consuming our time and resources.
The containment plan of the government states that in 2009, during the H1N1 Influenza pandemic it was observed that well connected big cities with substantive population movement were reporting large number of cases, whereas rural areas and smaller towns with low population densities and relatively poor road/ rail/ airway connectivity were reporting only few cases. It adds the current geographic distribution of COVID-19 mimics the distribution of H1N1 Pandemic Influenza. However, unlike 2009, India has now witnessed an unprecedented migration of labourers from cities to villages due to the lockdown. Do you agree that COVID19 will mimic H1N1 or do you think that due to the migration there will be hotspots in rural India? What will be the unique challenge, India would face, if the pandemic enters the villages?
I too believe that our large rural population will be relatively protected, if we are not lax in blocking urban to rural transmission. I have maintained, from the very beginning of our epidemic, that the large rural component and younger age of our population set us apart from the highly affected countries. I have confidence in the judgement of Dr Ravindran, Director of Emergency Medical Relief in the Health Ministry. He is a veteran who managed the response to the H1N1 epidemic and knows that pattern well. I believe that the reentry of poor migrants from urban areas in March would not have posed much threat as they were unlikely to have been exposed to returning foreign travellers or their contacts, due to the nature of their work and dwellings. However, we must now protect the villages from infection, by permitting only essential supplies and travel while ensuring availability of health and social protection services.
India has changed its testing strategy in the last four weeks. First, only those with travel and contact history were being tested. That has changed, and a wider spectrum of suspected patients are being tested. Now the ICMR has also allowed rapid antibody testing, not for the diagnosis, but for surveillance. First, has India tested enough? And second, how effective will be the rapid antibody testing, considering that a negative does not rule out the infection?
Most countries, including India, took time to define and initiate their testing strategy. The initial strategy was influenced by the assessed stage of the epidemic, the availability of testing labs and kits, the size of the total population as well as the groups identified to have a high probability of viral exposure.
Also Read | In zero-case Nanded, a worry: 4,000 stranded Punjab pilgrims
The strategy was progressively revised to expand testing labs, candidate criteria for testing and the type of tests. Since this was a new virus, there was a lag time in launching a high volume testing strategy initially. The antibody test seeks to identify a developed immune response in suspected cases and would be repeated after an interval if negative. Clinical features and exposure history would need to be taken into account while making the diagnosis and, where indicated, a viral antigen test may need to be performed in such antibody negative cases. The main use of the rapid test is to assess if a suspected case has acquired immunity to the virus and is safe for release from isolation.
Germany is thinking of issuing the ‘immunity passports’ for its key workers. Using the rapid antibody testing, researchers are preparing a list of key workers, who could be sent back to the workforce. Can India also identify such regions, wherewith the help of repeated testing we can ascertain the spread of the infection in localised area, and key workers can be sent back to the workforce?
This is a good strategy. India too should try it, to permit persons with acquired immunity to return to economically or socially productive work. How extensively this strategy can be deployed depends on the availability of kits and human resources to carry out large scale testing.
What do we know so far about the Indian strain of the virus? Is it as virulent as the strain found in Italy? How is aggressive is India working to develop a vaccine for the infection?
While some minor surface mutations have been reported in the viral strains isolated in India, there is no evidence yet of a change in behaviour related to virulence. We will know only as the epidemic evolves in the coming weeks. Even if there is no change in the character of the virus itself, expressed virulence is likely to be modified by the characteristics of the host (such as age and co-existing health conditions) as well as the environment (temperature and humidity). Vaccine development, in India, is being undertaken by Serum Institute and Zydus-Cadilla. A timeline of one year has been proposed for the vaccine.
With no specific drug therapies or vaccines, the USFDA announced a programme with “expanded access” to the treatment that uses transfusion of plasma from recovered patients to the severely ill. Should India also consider this experimental treatment?
This approach has been tried, in small non-randomised therapeutic trials, in China, South Korea, Singapore and USA. Passive antibody therapies were also tried earlier, in small numbers, in other viral diseases such as SARS and Ebola. A large randomised clinical trial of passive antibody therapy for COVID19, has just commenced in Canada. Pending the results of such trials, antibodies from plasma donated by recovered patients can be tried in seriously ill patients under the ‘compassionate use’ provision, if the treating medical team so decides.
Here’s a quick Coronavirus guide from Express Explained to keep you updated: What can cause a COVID-19 patient to relapse after recovery? | COVID-19 lockdown has cleaned up the air, but this may not be good news. Here’s why | Can alternative medicine work against the coronavirus? | A five-minute test for COVID-19 has been readied, India may get it too | How India is building up defence during lockdown | Why only a fraction of those with coronavirus suffer acutely | How do healthcare workers protect themselves from getting infected? | What does it take to set up isolation wards?
Apr 24: Latest News
- 01
- 02
- 03
- 04
- 05