Trending
This story is from October 17, 2020
Private medical sector should work with govt to save lives: GMC dean Bandekar
Goa’s battle chart for Covid moved from placid to stormy waters in a short span of three months and the Goa Medical College dean and head of Covid hospitals, Dr S M Bandekar, reckons the state will have to wait till December to see if the curve has flattened.

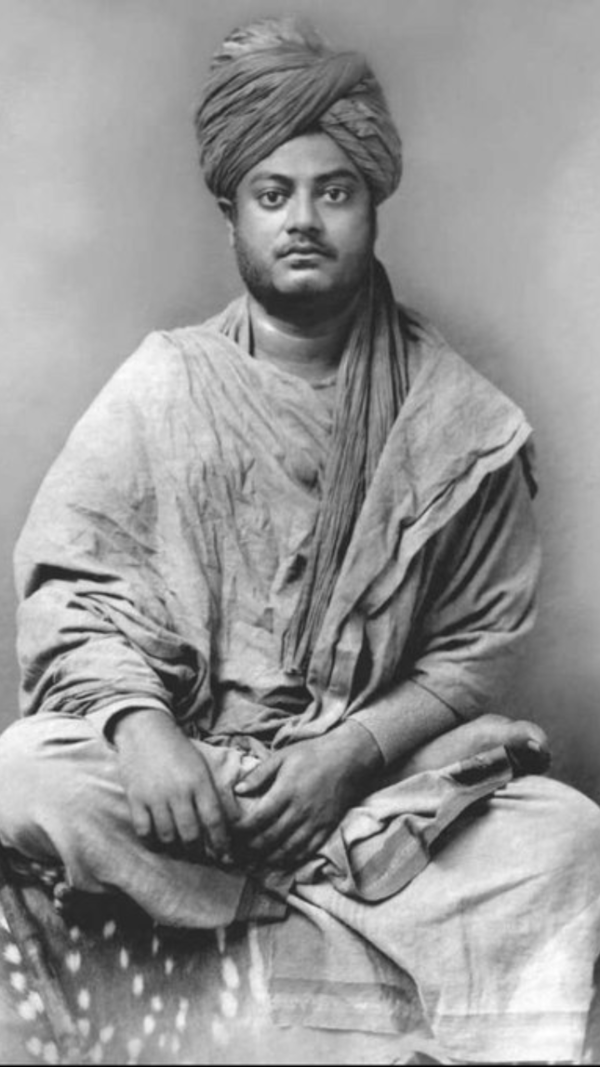
Goa Medical College dean and head of Covid hospitals, Dr S M Bandekar.
PANAJI: Goa Medical College dean and the head of Covid hospitals, Dr S M Bandekar, in an exclusive interview to TOI speaks about managing the epidemic in the state, the strategies in place and how he handled the psychological impact on patients and staff, as the state government struggled to meet infrastructural demands.
How are you managing with the increased caseload of Covid-19 with average daily admissions being 20-25?
We (at GMC) treat only critically critical patients.Non-critical Covid patients are either shifted to the ESI-Covid hospital or South Goa district hospital, which has been converted into a Covid hospital.
It must have been difficult to have beds that meet requirements of Covid patients in GMC due to lack of infrastructure? What do you do when suddenly the need for more beds is felt with rise in critical cases and some patients end-up on stretchers?

Do you plan to add more Covid beds?
Bed capacity of the South Goa district hospital is 500. If we utilise that capacity, we don’t think we will need more.
So, there is no need to have more beds for Covid patients in GMC?
The main purpose of GMC is to give critically ill patients the right care. All the 20-25 patients coming to GMC daily may not be critically ill. Some can be accommodated in the step down ICU and still some can be shifted to the South Goa district hospital. We have been managing in this fashion, but if cases rise, we may have to add more beds.

What is the biggest lesson you learnt from this unprecedented crisis?
Covid-19 has really shaken our whole set-up. Right from teaching to other services have been affected. Ours was the first medical college in the country to start online classes soon after the lockdown. But there is a lot of difference in online and actual teaching. Due to Covid-19, patients delayed their tertiary care treatment and refrained from coming to GMC. They thought they would contract the virus if they came to us. I do knee replacement surgeries, so I have seen several patients suffer, including a cancer patient since they deferred treatment. Non-reporting by patients is an important fallout of the virus.
At times, people told me that they feared even standing outside the GMC gate. Covid-19 is also the biggest social problem. There are lots of myths and misunderstandings about it. It affected the administrative set-up of the hospital. We had to convince people to come for work and on time. We counselled multi-task workers to work in wards where Covid patients are kept, repeatedly telling them that no harm will come to them if they wear protective gear and adequate precautions are taken. They are given protective personal equipment.
You were appointed to head Covid hospitals late, coinciding with a rise in infections in Goa. What was your biggest challenge then?
The biggest challenge was to reduce mortality rate. An expert committee to advise the government was appointed. We started with finding out what was the major cause for rise in mortalities. Also, a treatment advice committee was formed. We evaluated every day and went into details of cases and some things became clear. We modified infrastructure for treatment of Covid patients. The ICU beds were increased, and high flow nasal oxygen (HFNO) units were ordered.
Plus, we started patients on physiotherapy called “prone” which helps improve ventilation in the lungs. It has worked well. We also introduced psychological therapy for patients. Since patients remained in isolation and were not able to speak to anyone, some went into depression. More such cases were seen in the ESI-Covid hospital in the beginning. We have now occupational therapists visiting Covid wards, who work as counsellors. More importantly, we started a plasma mission to save lives.
Has it picked up?
Yes. A total of 444 patients have received plasma therapy so far and 90% have benefited from it. It must be understood that timing of the therapy is very important. If it is given within first three days of the patient showing the symptoms, results will be excellent. Ayush minister Shripad Naik and our director of health services were given plasma, and both recovered.
The government is under tremendous pressure to totally open GMC for Covid patients. Isn’t it a better option in managing the crisis?
We will open the entire medicine block of GMC with 500 beds for Covid patients if the need is felt. Two floors of the block are used for Covid patients. We never shied away from opening new wards for Covid patients. Almost every week we have added a new ward. We have 11 wards each having an average bed capacity of 25 for Covid patients.
If the need is felt, we will add more, but we cannot stop our tertiary care facility. Basically, we can’t turn down emergency cases. We have all major super specialities and combination of such facilities is difficult to find under one roof. Just because of Covid-19, treatment of cancer patients can’t be stopped. Delaying their treatment means denying it. Similarly, treatment can’t be refused to accident patients.
Considering the demand of non-Covid patients of Goa, we cannot think of converting the whole of GMC into a Covid hospital. If there was a parallel hospital as big as GMC, which could take off our load, then GMC could exclusively cater to Covid patients.
Till date the government has shouldered maximum responsibility towards Covid patients. The GMC is providing care for seriously ill patients, yet you have been at the receiving end. There is a malicious campaign against the GMC. Comment.
Right from the beginning, the government and the teams from GMC and the health services are trying their level best to give the best care to Covid patients. If people still have grievances against us, they can either come to the office of the dean or director of health services and state their objections rather than venting out their anger on social media or through any other medium.
The government is spending crores of rupees to give the best possible medical care to people. Yet some people may feel that proper care was not given to them in the public health facility. Even in countries with the best medical care, these issues exist.
All said and done, we can’t give personalised and 100% attention to all with our caseload being high. It is easier to manage if patient volume is less. We are doing our best like any other private health care facility.
What are your expectations from the private medical sector in the pandemic?
They should work shoulder-to-shoulder with the government. At times, we may not have a bed for a critical patient. In such times, patients should be able to avail treatment in private hospitals. Private doctors and we in the government set-up work to save lives. So, when we fall short of beds, they should fill the gap and save lives.
Is it true that in some patients Covid treatment may lead to aggravation of comorbid condition if any?
It is not entirely true. Covid patients are given steroids in the condition of cytokine storm, but it can increase blood sugar in a patient having diabetes. Such patients are not given steroids, only plasma therapy, so that their comorbid condition remains under control. It happens only in diabetic patients.
The government lost the first three precious months of the pandemic, which it could have used to build necessary infrastructure for Covid management, as it failed to foresee that the virus would escalate to this extent in Goa.
At the initial period of any pandemic, not much information is available about the disease in force. The same applies to Covid-19. So, I can’t say the government lost time, but it is true that we never faced this type of crisis in the past. Basically, we lacked experience during initial months in understanding how Covid-19 would pan out. We hardly had any cases till April-May and then suddenly cases rained.
What was your personal understanding of the pandemic at the beginning when you were not at the helm of affairs?
Looking at the kind of spread we saw in European countries and the US, we knew that Covid-19 was a very contagious disease. It leaves a disastrous effect on a patient’s respiratory system. Based on this information, we could have done something to tackle it, such as readied oxygen therapy units, installed more HFNO units.
Why is HFNO preferred in patient management in ICUs?
We know that oxygen therapy is the hallmark of Covid treatment. If a breathless patient is put on HFNO, his oxygen saturation level improves immediately. His recovery is faster if his lungs are cleared of infection. The HFNO is a better mode than having a patient on a ventilator support. Once a patient is on ventilator, chances of recovery lessen. HFNO and non-invasive ventilation are two important modalities that need to be used in patient management.
Should the government undertake sero survey at this stage?
Sero survey has meaning at the time of peak. It is done to gauge herd immunity in the population. I think we will have to wait.
So, you are saying we are not close to the peak?
I don’t think so because winter is yet to set-in. Even though winter in Goa is not harsh as elsewhere in the country, conditions of asthmatic patients worsens in December. So, we will have to wait to see the results.
Recently, the government released data that showed no significant variation in mortality rate six month prior to the pandemic and six months after. How would you read it?
There is no doubt that people are dying of pneumonia. But mortalities due to other causes have decreased. Now, we don’t have many cases of falciparum malaria. We have fewer dengue-related mortalities. We cannot deny Covid deaths. If the death count of the last and this year is compared, the numbers may tally. The reason being deaths caused due to high velocity accidents were reduced because of restrictions in place. Deaths occurring because of non-Covid causes may have lessened owing to one or more reasons and the gap is matched by Covid deaths. We need to have an exact number of pneumonia deaths from a total of mortalities reported though, in some cases, Covid-19 may be incidental.
When will GMC be able to restart its regular services?
We are still doing a lot of non-Covid work, but the magnitude of work is a little less than during normal times. As Covid cases decline, we will resume all our regular services, which may be either by the year-end or early next year.
How are you managing with the increased caseload of Covid-19 with average daily admissions being 20-25?
We (at GMC) treat only critically critical patients.Non-critical Covid patients are either shifted to the ESI-Covid hospital or South Goa district hospital, which has been converted into a Covid hospital.
It must have been difficult to have beds that meet requirements of Covid patients in GMC due to lack of infrastructure? What do you do when suddenly the need for more beds is felt with rise in critical cases and some patients end-up on stretchers?
We have the situation now under control. As of now there are no patients on stretchers. We have put additional beds in ward 113. So, if any patient needs to be given oxygen and there is no such bed free, we give him a bed in ward 113 and put an oxygen cylinder by his bedside.

Do you plan to add more Covid beds?
Bed capacity of the South Goa district hospital is 500. If we utilise that capacity, we don’t think we will need more.
So, there is no need to have more beds for Covid patients in GMC?
The main purpose of GMC is to give critically ill patients the right care. All the 20-25 patients coming to GMC daily may not be critically ill. Some can be accommodated in the step down ICU and still some can be shifted to the South Goa district hospital. We have been managing in this fashion, but if cases rise, we may have to add more beds.

What is the biggest lesson you learnt from this unprecedented crisis?
Covid-19 has really shaken our whole set-up. Right from teaching to other services have been affected. Ours was the first medical college in the country to start online classes soon after the lockdown. But there is a lot of difference in online and actual teaching. Due to Covid-19, patients delayed their tertiary care treatment and refrained from coming to GMC. They thought they would contract the virus if they came to us. I do knee replacement surgeries, so I have seen several patients suffer, including a cancer patient since they deferred treatment. Non-reporting by patients is an important fallout of the virus.
At times, people told me that they feared even standing outside the GMC gate. Covid-19 is also the biggest social problem. There are lots of myths and misunderstandings about it. It affected the administrative set-up of the hospital. We had to convince people to come for work and on time. We counselled multi-task workers to work in wards where Covid patients are kept, repeatedly telling them that no harm will come to them if they wear protective gear and adequate precautions are taken. They are given protective personal equipment.
You were appointed to head Covid hospitals late, coinciding with a rise in infections in Goa. What was your biggest challenge then?
The biggest challenge was to reduce mortality rate. An expert committee to advise the government was appointed. We started with finding out what was the major cause for rise in mortalities. Also, a treatment advice committee was formed. We evaluated every day and went into details of cases and some things became clear. We modified infrastructure for treatment of Covid patients. The ICU beds were increased, and high flow nasal oxygen (HFNO) units were ordered.
Plus, we started patients on physiotherapy called “prone” which helps improve ventilation in the lungs. It has worked well. We also introduced psychological therapy for patients. Since patients remained in isolation and were not able to speak to anyone, some went into depression. More such cases were seen in the ESI-Covid hospital in the beginning. We have now occupational therapists visiting Covid wards, who work as counsellors. More importantly, we started a plasma mission to save lives.
Has it picked up?
Yes. A total of 444 patients have received plasma therapy so far and 90% have benefited from it. It must be understood that timing of the therapy is very important. If it is given within first three days of the patient showing the symptoms, results will be excellent. Ayush minister Shripad Naik and our director of health services were given plasma, and both recovered.
The government is under tremendous pressure to totally open GMC for Covid patients. Isn’t it a better option in managing the crisis?
We will open the entire medicine block of GMC with 500 beds for Covid patients if the need is felt. Two floors of the block are used for Covid patients. We never shied away from opening new wards for Covid patients. Almost every week we have added a new ward. We have 11 wards each having an average bed capacity of 25 for Covid patients.
If the need is felt, we will add more, but we cannot stop our tertiary care facility. Basically, we can’t turn down emergency cases. We have all major super specialities and combination of such facilities is difficult to find under one roof. Just because of Covid-19, treatment of cancer patients can’t be stopped. Delaying their treatment means denying it. Similarly, treatment can’t be refused to accident patients.
Considering the demand of non-Covid patients of Goa, we cannot think of converting the whole of GMC into a Covid hospital. If there was a parallel hospital as big as GMC, which could take off our load, then GMC could exclusively cater to Covid patients.
Till date the government has shouldered maximum responsibility towards Covid patients. The GMC is providing care for seriously ill patients, yet you have been at the receiving end. There is a malicious campaign against the GMC. Comment.
Right from the beginning, the government and the teams from GMC and the health services are trying their level best to give the best care to Covid patients. If people still have grievances against us, they can either come to the office of the dean or director of health services and state their objections rather than venting out their anger on social media or through any other medium.
The government is spending crores of rupees to give the best possible medical care to people. Yet some people may feel that proper care was not given to them in the public health facility. Even in countries with the best medical care, these issues exist.
All said and done, we can’t give personalised and 100% attention to all with our caseload being high. It is easier to manage if patient volume is less. We are doing our best like any other private health care facility.
What are your expectations from the private medical sector in the pandemic?
They should work shoulder-to-shoulder with the government. At times, we may not have a bed for a critical patient. In such times, patients should be able to avail treatment in private hospitals. Private doctors and we in the government set-up work to save lives. So, when we fall short of beds, they should fill the gap and save lives.
Is it true that in some patients Covid treatment may lead to aggravation of comorbid condition if any?
It is not entirely true. Covid patients are given steroids in the condition of cytokine storm, but it can increase blood sugar in a patient having diabetes. Such patients are not given steroids, only plasma therapy, so that their comorbid condition remains under control. It happens only in diabetic patients.
The government lost the first three precious months of the pandemic, which it could have used to build necessary infrastructure for Covid management, as it failed to foresee that the virus would escalate to this extent in Goa.
At the initial period of any pandemic, not much information is available about the disease in force. The same applies to Covid-19. So, I can’t say the government lost time, but it is true that we never faced this type of crisis in the past. Basically, we lacked experience during initial months in understanding how Covid-19 would pan out. We hardly had any cases till April-May and then suddenly cases rained.
What was your personal understanding of the pandemic at the beginning when you were not at the helm of affairs?
Looking at the kind of spread we saw in European countries and the US, we knew that Covid-19 was a very contagious disease. It leaves a disastrous effect on a patient’s respiratory system. Based on this information, we could have done something to tackle it, such as readied oxygen therapy units, installed more HFNO units.
Why is HFNO preferred in patient management in ICUs?
We know that oxygen therapy is the hallmark of Covid treatment. If a breathless patient is put on HFNO, his oxygen saturation level improves immediately. His recovery is faster if his lungs are cleared of infection. The HFNO is a better mode than having a patient on a ventilator support. Once a patient is on ventilator, chances of recovery lessen. HFNO and non-invasive ventilation are two important modalities that need to be used in patient management.
Should the government undertake sero survey at this stage?
Sero survey has meaning at the time of peak. It is done to gauge herd immunity in the population. I think we will have to wait.
So, you are saying we are not close to the peak?
I don’t think so because winter is yet to set-in. Even though winter in Goa is not harsh as elsewhere in the country, conditions of asthmatic patients worsens in December. So, we will have to wait to see the results.
Recently, the government released data that showed no significant variation in mortality rate six month prior to the pandemic and six months after. How would you read it?
There is no doubt that people are dying of pneumonia. But mortalities due to other causes have decreased. Now, we don’t have many cases of falciparum malaria. We have fewer dengue-related mortalities. We cannot deny Covid deaths. If the death count of the last and this year is compared, the numbers may tally. The reason being deaths caused due to high velocity accidents were reduced because of restrictions in place. Deaths occurring because of non-Covid causes may have lessened owing to one or more reasons and the gap is matched by Covid deaths. We need to have an exact number of pneumonia deaths from a total of mortalities reported though, in some cases, Covid-19 may be incidental.
When will GMC be able to restart its regular services?
We are still doing a lot of non-Covid work, but the magnitude of work is a little less than during normal times. As Covid cases decline, we will resume all our regular services, which may be either by the year-end or early next year.
End of Article
FOLLOW US ON SOCIAL MEDIA