Excellence in Nursing Awards 2021
Meet this year's 13 outstanding nurses
When you think “Greatest Nurse of All Time,” Florence Nightingale might come to mind. But comparing today’s modern nurses to the famous one of the 19th century doesn’t give our nurses the credit they deserve. Since Nightingale founded the first nursing school in 1860 at St Thomas’ Hospital in London, the nursing profession has come a long way.
Today’s nurses are highly skilled and integral healthcare partners in modern medicine. Recent events reminded the world of just how often nurses are the unsung heroes of the medical community. These talented individuals provide their skills and sacrifice on a daily basis, and now, thanks to COVID-19, we have a glimpse of the debt we owe.
New Hampshire Magazine, in partnership with the New Hampshire Nurses Association, is proud to highlight nurses’ important contributions with the annual Excellence in Nursing Awards. This past winter, we accepted nominations for New Hampshire nurses in 13 vital specialties, from pediatrics and public health to leadership and education. The winners were selected by an independent committee of nursing leaders from adjoining states. Each nurse profiled in the following pages represents the very best in nursing — those who go above and beyond to comfort, heal and teach.
Meet this year’s award-winning nurses:
Erin St. Gelais, BSN, RN-BC, CPAN
Margaret Georgia, MBA, BSN, RN, CCM
Jennifer Krueger, BSN, RN, CPN
Evie Stacy, MS, APRN
Polly Campion, MS, RN
Jamye Cutter, BSN, RN
Janet Carroll, RN, CEN, SANE-A, SANE-P
Jennifer Pletcher, MPH, BS, RN, CEN, PhD Candidate
Jillian C. Belmont, DNP, FNP, AGACNP, SCRN
John T. Flynn, RN, BSN
Judith Joy, PhD, RN
Lisa Wesinger, RN, BSN, OCN, BMTCN
Catherine Oliver, BSN, RN

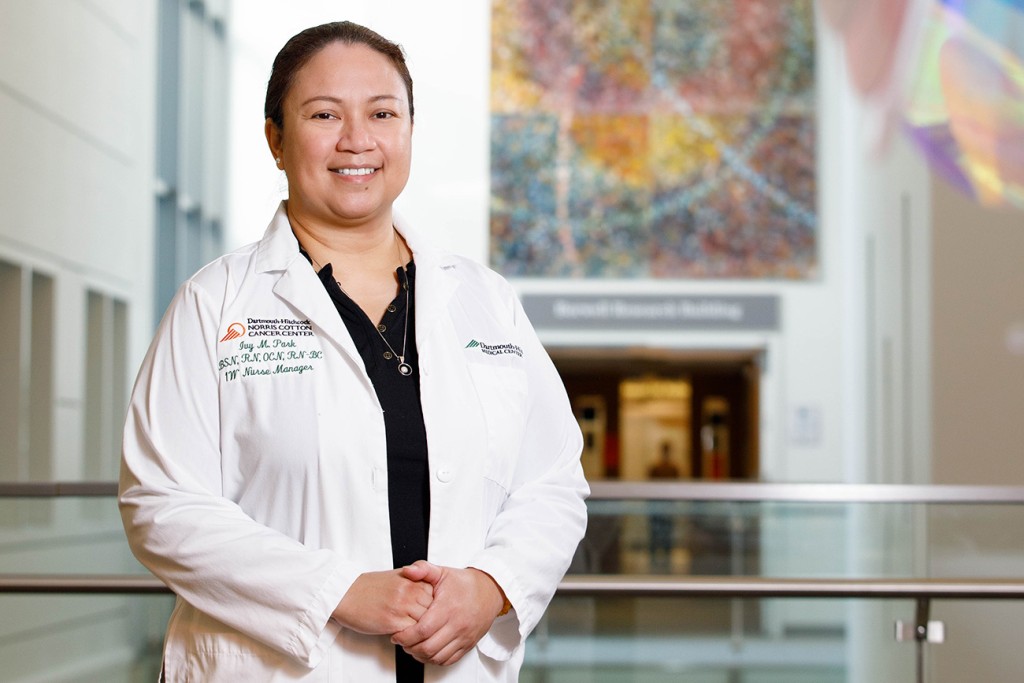
Erin St. Gelais, BSN, RN-BC, CPAN Photo by Kendal J. Bush
Erin St. Gelais, BSN, RN-BC, CPAN
Medical-Surgical Nursing
Wentworth-Douglass Hospital
Working in a post-anesthesia care unit (PACU) requires flexibility, compassion and critical thinking, says Erin St. Gelais. “You never know what will come through the door, how a person will wake up, what their recovery will be or what their needs are,” she says. “You have to learn to anticipate needs and critically think your way through cases. And like any nursing discipline, it takes a lot of compassion.”
She started working as a registered nurse at Wentworth-Douglass Hospital in 2005 and joined the PACU team in 2012, where she cares for patients recovering from anesthetics. There are many parts to her job, but “having the ability to make people more comfortable and contribute to taking away pain after a procedure is a very rewarding part,” she says.
Though this past year was difficult, St. Gelais focuses on the inspiring people who rose to the occasion.
“We all see stories that have been coming out of the pandemic of frontline workers, first responders, even retired healthcare workers coming back to help out in any way for tireless hours to care for those in need no matter the circumstances just because there was a need,” she says. “A lot of those we care for are pretty amazing and have some pretty inspiring stories if you listen.”

Margaret Georgia, MBA, BSN, RN, CCM Photo by Kendal J. Bush
Margaret Georgia, MBA, BSN, RN, CCM
Senior Nursing Leader
Dartmouth-Hitchcock Medical Center
As director of care management for Dartmouth-Hitchcock, Margaret Georgia, by definition, plays a critical role in the care given to patients, but like everything during the past year of pandemic, the stakes have increased.
“I oversee a department that is responsible for care coordination and discharge planning,” says Georgia, who has been a nurse for 40 years. Determining and guiding the steps for the timely release from the hospital involves more than just a happy ending to a patient’s stay, it affects the work of everyone else in the facility. “If we don’t discharge patients, we don’t have capacity to admit new patients who need our care,” she says.
Facilitating communications between patients, families and teams of health care providers internally and out in the community requires strong critical thinking skills to solve the problems that pop up in hospital settings. “You have to be organized and able to juggle many things at the same time,” says Georgia. “Above all, you have to have integrity and be a patient advocate,” she says, and especially in a time when the role of a patient’s family is more of a challenge due to quarantine restrictions.
Georgia recalls a serendipitous admission to the hospital she endured while a student in nursing school: “I experienced from a patient’s perspective what a difference a nurse can make at a most vulnerable time in someone’s life.” It might also help that she comes from a “long line of nurses” in her family. “My mother and two of her sisters were or are nurses as well as many cousins,” she says. “I strive to meet the standards that they set for all of us.”

Jennifer Krueger, BSN, RN, CPN Photo by Kendal J. Bush
Jennifer Krueger, BSN, RN, CPN
Pediatric and School Nursing
Elliot Hospital
After finishing nursing school in 2013, Jennifer Krueger spent time in the float pool at Elliot Hospital, working in various units. While she’s grateful for the wide range of skills she gathered along the way, when she arrived in the pediatric unit, she knew her floating days were done.
“My patients are what make me strive for excellence in nursing,” says Krueger, who is now the resource nurse on the pediatric unit, meaning she’s usually the charge nurse and is a part of the leadership team, helping her coworkers with their patients and managing the unit during her shifts.
“Hospitalizations are stressful for both the child and their family,” says Krueger. “It is very rewarding to be able to make a positive impact for them during a difficult time.”
During her first winter on pediatric unit, a boy — who happened to be the same age as her daughter at the time — was in her care. “This hospitalization was especially difficult for his mom,” says Krueger, who ended up helping both mom and son through a stressful time. “This family had a big impact on me, and taught me the importance of caring for not only the patient but also the family,” she says.
No one wants to find themselves in a hospital, but it can be extra overwhelming and frightening for children. Luckily, Krueger understands what kids need.
“I feel that patience is an extremely important characteristic for nurses in pediatrics,” she says.
“It takes time to build trust with a child to help them feel comfortable with the care you are providing. Something as simple as giving medication can cause a lot of stress for a child. Being patient with them and adjusting your approach to their needs can help ease their fears.”

Evie Stacy, MS, APRN Photo by Kendal J. Bush
Evie Stacy, MS, APRN
Psychiatric and Mental Health Nursing
Dartmouth-Hitchcock Clinic
Like many health care providers, Evie Stacy felt the impact of the pandemic. As a pediatric nurse practitioner and child/adolescent psychiatric nurse practitioner in the Embedded Psychiatry Department at Dartmouth-Hitchcock Manchester, she’s helped young people deal with a scary new world.
“Life has been turned upside down with the loss of routine and the lack of social interactions with peers,” says Stacy. Anxiety and depression are on the rise, she says, as “families are struggling with loss of jobs, financial stress or parents trying to work from home. Remote schooling presents significant challenges as well, and it causes increase in anxiety for all members of the family.”
But Stacy is equipped to help young people through these unprecedented challenges. After working in community mental health with the mentorship of a child psychiatrist, she returned to graduate school at Boston College, learning more about mental health/psychiatric nursing.
“The most important aspect in providing mental health care is to carefully listen to the child or adolescent,” says Stacy. “I encourage honesty, as there are no right or wrong answers to my questions. Developing a therapeutic and respectful relationship allows me to provide more
effective care.”
She’s put her skills to good use over the years, helping young people grow and mature. She recalls a college student who was dealing with significant anxiety. As he was about to graduate, he invited Stacy to his senior art show, letting her know her support was crucial to his success. “It was an honor to attend,” she says. And then there was the young man in middle school with Tourette’s disorder. His vocal and motor tics were so severe they prevented him from attending classes. He’ll be graduating from college next year.

Polly Campion, MS, RN Photo by Kendal J. Bush
Polly Campion, MS, RN
Public Health Nursing
NH State Commission on Aging, Former state legislator
Polly Campion’s interest in public health began with a stint as a VISTA volunteer assisting a nurse practitioner and a mobile medical van with well-child exams in rural Vermont. Or maybe it began with her mom, who was a lifelong public health nurse, “always seeking to connect community members with resources,” recalls Campion. Nurses seem to find their callings early in life.
After a career detour into elementary education, Campion returned to nursing to work for 24 years at Dartmouth-Hitchcock Medical Center and to serve four years as a NH state legislator.
This last role, along with roles in organizations such as the NH Health Care Quality Assurance Commission, where she was the inaugural chair, have allowed her to perform the most important single skill of a public health specialist: “Advocacy,” she says.
The ability to see the big picture while learnng of the details of individual experiences is the gift of the advocate, says Campion. “Know that systems and processes influence individual actions, successes and challenges,” she says. “Then use that perspective to create policy changes and improve systems of care.”
Campion currently chairs the NH State Commission on Aging and participates in the COVID-19 Senior Support Team as regional coordinator. And she continues, above all, to advocate for patients, groups and the greater Granite State.

Jamye Cutter, BSN, RN Photo by Kendal J. Bush
Jamye Cutter, BSN, RN
Maternal-Child Health Nursing
Granite VNA
“I’ve had the privilege of meeting so many families facing difficult times ahead, and it is their resilience and courage that keeps me motivated to be a better nurse, grow in my career, and meet the needs of my community,” says Jamye Cutter.
As a pediatric nurse, Cutter provides skilled nursing care in the home to maternal child health parents. “I do new mom and baby visits, IV therapy, chemo, assessments of infants and children, and anything else that you can think of that relates to nursing,” she says. “I also coordinate community resources and work with area agencies on a regular basis. I provide support and education to families regarding medical diagnoses and infant growth and development.”
Cutter has devoted her life and career to caring for women and children. During her career, she’s learned that there isn’t any single key to success. “Compassion, integrity and honesty are all vital to providing excellent care to families,” she says. “The families that I serve are at one of the most vulnerable times in their lives. They may be welcoming a new baby into the home and trying to adapt or they may be facing the death of a child and need guidance and support.”
As hard as the work may be at times, Cutter is buoyed by her patients, especially by the special reminders they’ve sent her over the years, like the Christmas tree ornaments she holds dear. “Each ornament carries a memory,” she says.
“One ornament was handed to me as I walked out of their home for the last time,” she recalls.
“Even though it had been a mere few hours after hearing her baby’s heartbeat for the last time, that mom thought of me, and wanted to give me something to always remember her baby. Each ornament, its own journey, with a special place in my heart.”

Janet Carroll, RN, CEN, SANE-A, SANE-P Photo by Kendal J. Bush
Janet Carroll, RN, CEN, SANE-A, SANE-P
Emergency Nursing
Nurse Manager, Forensic Nursing Program and NH SANE Program Co-director
Dartmouth-Hitchcock Medical Center and NH Coalition Against Domestic and Sexual Violence
Janet Carroll has worked as a registered nurse for 21 years, primarily in the emergency department. She began specializing in forensic nursing in 2005, and currently works in that field, providing specialized medical forensic care to patients who have experienced acts of violent crime such as sexual assault, physical assault, strangulation, gunshot wounds, domestic violence, human trafficking and more.
It’s crucial, says Carroll, to remain “calm, nonbiased and nonjudgmental in the midst of controlled chaos.” She is inspired to be the best nurse she can by both the patients she treats and her family of colleagues.
In addition to her work at Dartmouth-Hitchcock, Carroll works part time with the NH Coalition Against Domestic and Sexual Violence. She is co-director for the New Hampshire Sexual Assault Nurse Examiner program (SANE), a group of nurses who trained to provide comprehensive care to sexual assault survivors, including conducting forensic evidence collection.
SANE’s goal is to help victims by minimizing both physical and psychological trauma while ensuring that physical evidence is properly collected and preserved.
“I never thought of getting into forensic nursing until I was working a night shift and a woman came into the emergency department reporting sexual assault,” says Carroll. It was a busy evening in the ER, and combined with short staffing the woman “did not get the one-on-one care she needed and deserved,” she says. “It was [at] that moment that I decided to further explore forensics, and it has expanded from there.”

Jennifer Pletcher, MPH, BS, RN, CEN, PhD Candidate Photo by Kendal J. Bush
Jennifer Pletcher, MPH, BS, RN, CEN, PhD Candidate
Nurse Educator/Researcher
Concord Hospital
Given that Jennifer Pletcher is this year’s winner in the nurse educator/researcher category, it’s not surprising that she identifies the “tenacity to always ask why, followed by the commitment to get to the truth of the answer” as the most important trait for someone in her field.
From the outside, it appears that her ability to multitask is just as important to her success.
Pletcher works both clinically and as an educator in the ER at Concord Hospital, collects data to evaluate the hospital’s stroke care process, and is working on her dissertation, which is focused on ER visits exacerbated by substance use disorder and how nurses can help navigate this increasingly complicated situation.
For Pletcher, education, research and making evidenced-based changes are how the health care system will improve to better serve patients no matter their circumstances. Throughout her career, she’s traveled the country and witnessed the disparities that exist in health care. During an internship with James Vara, Gov. Sununu’s commissioner for substance use disorders and mental health, “there was a tangible, palpable connection between evidence, or lack of evidence, shaping policy to best advocate for patients and patient care,” she says.
These experiences exposed some of the flaws in the system, but she’s not discouraged. “There are so many difficult ‘problems’ within health care, which are sometimes overwhelming,” she says, but by focusing on the small victories she’s inspired to keep trying.
When a patient arrived in the ER with an injection site infection due to substance abuse disorder, she asked him and his significant other if they had access to Narcan, a potential life-saver in the case of opioid overdose. Both, says Pletcher, looked at her in shock — simply because “I was seeing him as a human being worthy of assistance in his life course as he pursued his own definition of health,” she says.
“The fact that this patient was surprised to be treated with dignity inspires me to push forward, break molds, educate other nurses, and provide data with analyses through research in hope that one day, regardless of patient health or socioeconomic status, being treated human is never a surprise.”

Jillian C. Belmont, DNP, FNP, AGACNP, SCRN Photo by Kendal J. Bush
Jillian C. Belmont, DNP, FNP, AGACNP, SCRN
Advanced Practice Nursing
Lead Associate Provider, Neurology, Co-director, Neurology Advanced Practice Provider Fellowship, Assistant Professor in Neurology, Geisel School of Medicine
Dartmouth-Hitchcock Medical Center
Understanding her “why” is Jillian Belmont’s key to success, a trait she also sees in her talented colleagues.
“Every day I am inspired by their knowledge, collegiality, their passion and their constant fight alongside patients, which leads to limitless learning and elevation of those around them,” she says. “I show up to work every day and I know my ‘why.’ When I look around at my peers, they undoubtedly are showing up to work every day with an understanding of their ‘why.”’
One of the most important things she’s learned is to never take anything for granted.
“You never know how much time, how many days or even the number of breaths you may have left,” she says. “As I learned very quickly in nursing, life can change very quickly and without notice. Never take a day, a moment or opportunity for granted.”
Belmont started her career in 2008 as a bedside nurse. She continued working full time while pursuing a master’s degree and family nurse practitioner certification, kickstarting her career as a neurology NP in 2012 at Dartmouth-Hitchcock Medical Center. In 2017, she received a doctorate in nursing practice from Northeastern University.
A year later, she obtained her adult geriatric and acute care NP certification. Now she works as a neurology nurse practitioner and serves as co-director of DHMC’s neurology Advanced Practice Provider post-graduate fellowship, president of the local American Association of Neuroscience Nursing chapter and president of the New Hampshire Nurse Practitioner Association.
Though Belmont’s years of education and professional growth speak to a strong work ethic and desire to always learn more, she says that the most important skills for someone in her field are “compassion, respect and resilience.”

John T. Flynn, RN, BSN Photo by Kendal J. Bush
John T. Flynn, RN, BSN
Cardiovascular Nursing
Lead Associate Provider, Neurology
Dartmouth-Hitchcock Medical Center
For John Flynn, it’s all about kindness, all the time.
“Fred Rogers shared the three ways to ultimate success. The first way is to be kind. The second way is to be kind. The third way is to be kind,” Flynn says. “I am surrounded by kind and dedicated caregivers. They inspire me with every life-saving class to promote team care of each other and our patients, within moments of emergencies.”
Flynn is a cardiology nurse in the cardiac catheterization laboratory (cath lab) at the Dartmouth-Hitchcock Heart & Vascular Center, where he’s worked since 2005. Before working in the field of cardiology, he was a nurse at the Children’s Hospital at Dartmouth (CHaD).
Each week, he teaches both adult and child advanced life support classes with members of the DHMC team.
In addition to coworkers and patients, Flynn finds inspiration in Mother Teresa. He often references her quote, “I can do things you cannot, you can do things I cannot: Together we can do great things.” To Flynn, her message emphasizes the importance of teamwork in order to provide kind care to his patients.
“In our cath lab, emergent team care is delivered in seconds, every day, with clear team roles. The healing outcomes are the combination of our kindness to each other and the reverence to needing each other,” he says.

Judith Joy, PhD, RN Photo by Kendal J. Bush
Judith Joy, PhD, RN
Front Line/Administrative Nursing Leader
Front Line/Administrative Nursing Leader at NH COVID Alliance Senior Support Team, Volunteer Statewide Coordinator
For Judith Joy, working in elder care is both challenging and fulfilling, especially during COVID-19. When the pandemic hit, she was recruited to be the statewide lead for the NH COVID Alliance Senior Support team, a multidisciplinary remote team that supports senior care facilities. Joy and her team recruited volunteers from groups such as the New Hampshire Nurses and School Nurses associations, and together monitored facilities daily in an effort to reduce outbreaks.
The success of the program can be attributed to the diverse experience of the volunteers, says Joy — but strong leadership is crucial as well. Listening, she says, is one of the essential qualities for any leadership role. “Listening supports effective decisions, helping to determine when and from whom to seek input,” she says.
Inspiration comes both from her role as a leader and from her associates. “My nursing colleagues throughout my career have encouraged me to continue growing in formal education and experience,” she says. “I owe them any success I might have.”

Lisa Wesinger, RN, BSN, OCN, BMTCN Photo by Kendal J. Bush
Lisa Wesinger, RN, BSN, OCN, BMTCN
Ambulatory Care Nursing
Blood and Marrow Transplant/Cellular Therapy Nurse Navigator
Dartmouth-Hitchcock Medical Center-Norris Cotton Cancer Center
Each patient holds a special place in Lisa Wesinger’s heart.
One in particular stays with her. A man undergoing cancer treat-ments created a “Ken Burns-like” movie of happy memories from his life, with characters portraying the disease as dark, villainous skeletons, and a superhero named “Captain Chemo” fighting the battle for him. He had hoped to eventually share the movie with his medical team, but his disease progressed rapidly, moving up the timeline. “I was able to honor his final wishes and packed an auditorium with over 70 people. He sat at the top of the room and proudly watched the reactions of the audience — there was not a dry eye to be had,” Wesinger says.
Wesinger spent the first 21 years of her career working as a hematology special care nurse at Dartmouth-Hitchcock Medical Center. In 2019, she transitioned to the blood and marrow transplant clinic team, working as a blood and marrow/transplant cellular therapy nurse navigator. Her responsibilities include guiding patients and their families through the complexities of stem cell transplant and CAR T-cell therapy.
“Being committed to the patients and caregivers and developing trusting relationships is very important in my specialty,” says Wesinger.
Although it’s never easy to watch people undergo such arduous medical battles, Wesinger’s patients “inspire me each and every day,” she says. “Patients facing a cancer diagnosis need to be strong and stay strong. Every day they deal with the uncertainty of what the next day brings. We provide hope and fight right along with them.”

Catherine Oliver, BSN, RN Photo by Kendal J. Bush
Catherine Oliver, BSN, RN
Hospice-Palliative Care and/or Gerontologic Nursing
Nurse Manager Community Living Center (CLC)
Manchester VA Medical Center
Catherine Oliver’s first job as a nursing assistant at the New Hampshire State Hospital was the kind that tests the resolve of new nurses, often leading them to pursue other careers — but not Oliver. She joined the military, went to school and graduated from New Hampshire Technical Institute in 1999, and started working for the VA Medical Center, where she has remained in the same unit for over 20 years serving rehab veterans and veterans at end of life.
For motivation, Oliver looks to her family and mentors.
“Susan Roswell gave me a great foundation to grow from; Jen Winslow has mentored me and taught me professional etiquette; and Dr. Moscola shared her vast knowledge with me to ensure everything that we do is evidence-based practice. I wouldn’t be where I am today without any of them.”
You need patience and compassion as a nurse, but you also need a sense of humor, she says. “I am always looking for ways to improve the veteran experience and give them the highest quality of life possible,” she says. “Humor and making someone laugh are great ways to accomplish that. Our veterans and families are happy because the staff here have improved their lives for the better, from the simple task of cutting their hair to providing exceptional end-of-life care. We smile because they do.”