By Clarissa Donnelly DeRoven, North Carolina Health News
At 9 a.m. the meeting begins.
“Would you spend the night in a haunted house?” Liz, a participant in the day program at Hinds’ Feet Farm in Asheville, asks her fellow group members, who sit scattered at round tables throughout the room.
She answers her own question first: a firm no. No explanation needed.
Jason, Liz’s fiance, answers next. He says he would. Sam, another participant, goes after. He hems and haws for a moment.
“Well, I’d have to bring my CPAP so …” he trails off. Someone else echoes the concern: they, too, would need to bring their CPAP into the haunted house. The group bursts into laughter.
A CPAP, or continuous positive airway pressure, is a machine used to treat sleep apnea, a type of sleep disturbance common for people with brain injuries, the exact clientele who make up the day program at Hinds’ Feet Farm. The agency serves those with brain injuries stemming from all causes, both traumatic brain injuries — for example from a fall, or a car accident — or non-traumatic injuries, such as from a stroke, or oxygen deprivation.
Part of the joy for members of the program is the community, the easy feeling they get being around other people who understand what it’s like to live with a brain injury. These are folks who don’t need an explanation for what a CPAP machine is or why you might need one, but who will simply laugh at the thought of lugging the thing into a spooky old house.
Valuing ‘quality of life’ more than ‘recovery’
Many adults with disabilities spend time in day programs. They can help participants strengthen a variety of skills, depending on their needs. In all of North Carolina, there are just three day programs specifically for people with brain injuries. Hinds’ Feet Farm runs two of them year round, Monday through Thursday, from 9 a.m. to 3 p.m. Many participants come every day.
The organization gained official non-profit status in 2001, opening its first location on a farm in Huntersville, outside of Charlotte. The Asheville location, high up on a hill, opened in 2009. It rents rooms from the Asheville Foster Seventh-day Adventist Church on Hendersonville Road. While the name of the agency is biblical, and the founders have explained their draw toward the work as based in Christian principles, all the programming is secular and people of all (and no) faiths are welcome.
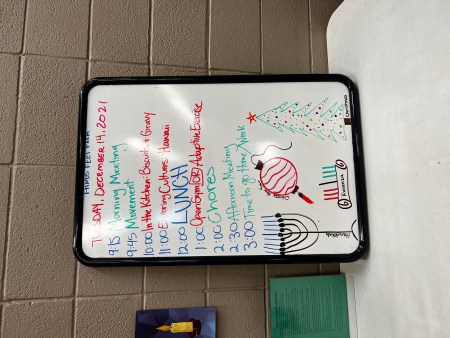
In Asheville, the day starts with a meeting, usually an icebreaker — “Would you spend the night in a haunted house?” for example — some body movement, then onto activities: perhaps a cooking class or card games, followed by an educational session, lunch, time to exercise, onto chores and a goodbye meeting.
The schedule is flexible. It’s designed in collaboration with the participants. Each month, they meet and discuss what they want to learn, practice and focus on during the following month. The program coordinators then create a schedule that brings all those desires together.
Collaborative programming that focuses on social-emotional health has always been the goal of Hinds’ Feet. The organization’s genesis lies in 1984 when executive director Marty Foil’s 16-year-old brother Philip suffered a traumatic brain injury in a car accident. Once Philip completed medical treatment — his hospital stay, in-patient and out-patient rehab — the family came to a disturbing discovery: they couldn’t find any services to help him keep up the gains he’d made in rehab, or to help him reintegrate into society after his injury.
The Foils decided they’d create a program to fill the gap.
“We didn’t understand the linguistics and the language” of the behavioral health system, Foil said. “All we knew, conceptually, is that we wanted to develop programming that would maximize somebody’s quality of life.”
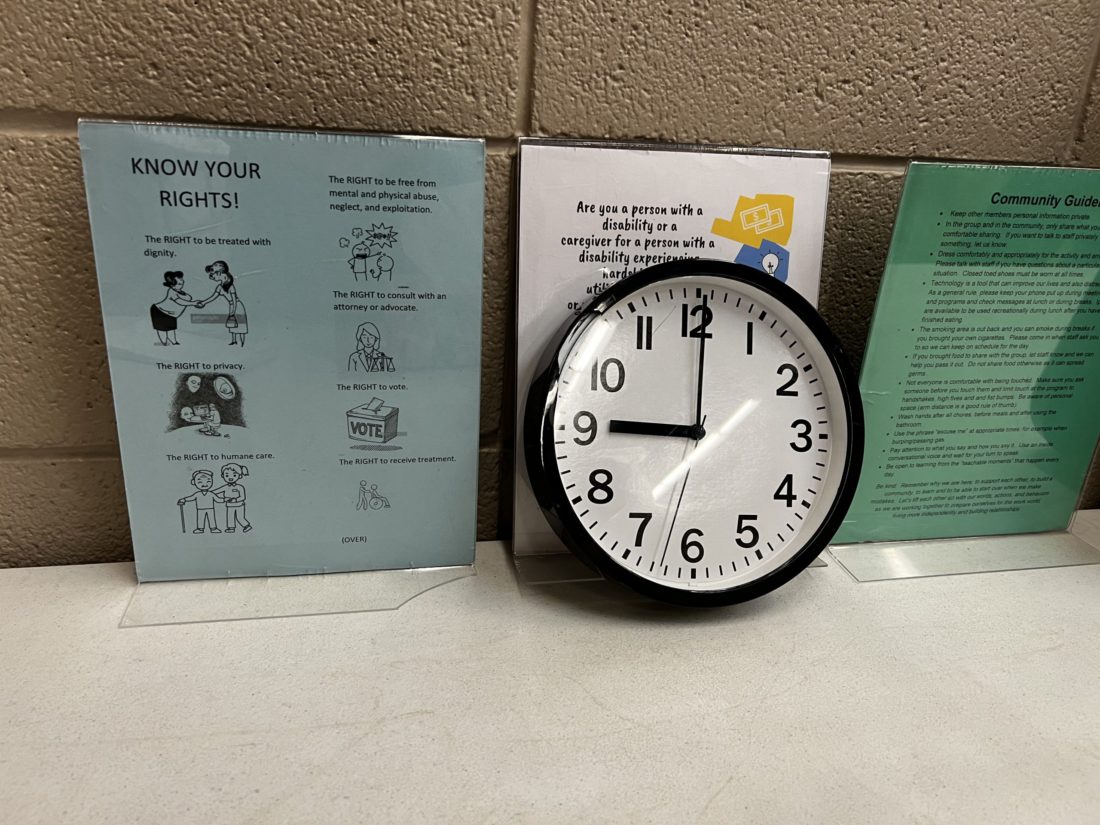
They wrote their mission statement with that in mind: “To maximize the post injury potential of persons living with brain injury with integrated, unique, and holistic programs; allowing our members to pursue meaningful activities while developing a sense of belonging at home and in the surrounding communities.”
Foil, and staff at the Asheville location, make clear that the organization’s goal has not and will never be to help people with brain injuries “get better.” Brain injuries are unique, and everybody’s level and pace of recovery looks different. The program is designed to meet people where they are, and help them achieve personal goals within the new reality their injury has placed them in.
Personal goals met
One of Liz’s goals, for example, is to give tours to new visitors. Accompanied by Jason, who pushes her wheelchair, and day program director Erica Rawls, she practices on me. Many people who have brain injuries struggle with short-term memory, and so for ethical and privacy reasons NC Health News is using only participant’s first names.
We exit the main room, where the icebreaker took place, and enter a hallway. Sprouting off the hallway are smaller rooms where breakout groups or individual meetings happen, and another room that belongs to a different non-profit.
Jason gestures to the end of the hallway. “The gym is over there too, isn’t it?” he says.
“She’s not there yet,” Rawls reminds him. “We’re going to let Liz take the lead.”
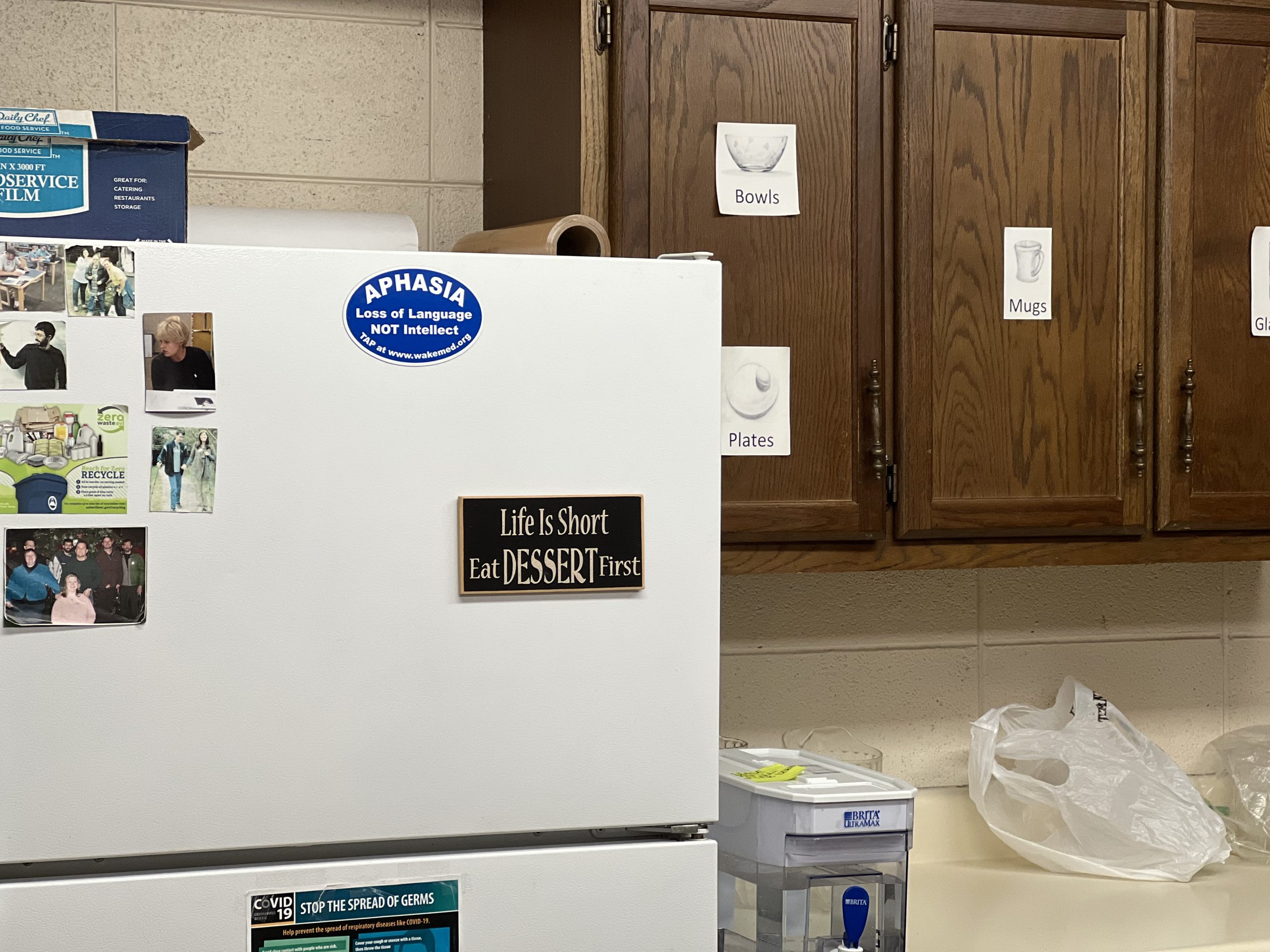
From her brain injury, Liz has aphasia, a language disorder that can manifest in various ways for different people. For her, it means she speaks slowly. Jason also has a brain injury, but he does not speak slowly.
“Okay, okay, okay,” Jason says, quickly. He gives Liz a kiss on the head.
“No! We can’t do that here,” Liz says, and giggles.

Rawls smiles. “We’re giving each other space while we’re at the program, right?” she says. “Did you want to talk about the gym before we leave this area?”
Liz says yes, and we continue the tour.
Opposite the direction of the gym is the kitchen. Today, Liz will lead a cooking class, where she’ll teach the other participants how to make biscuits and gravy. Down the other hallway is the outdoor smoking area, and a small garden the members tend to during warmer months. The growing area used to be in beds on the ground, but after receiving a grant the organization recruited a student from Warren Wilson College to put the beds up on legs so people in wheelchairs could participate.
“I used to not be able to garden,” Liz explains, as she rolls her chair under the garden’s raised edge, “but now I can.”
Underfunded home and community-based services
The federal Centers for Disease Control and Prevention estimates that about 2% of the population lives with a disability caused by a traumatic brain injury. In North Carolina, that means as many as 200,000 people. Despite the high number, those in the field argue that funding for care has long lagged. The state Department of Health and Human Services only began specifically funding TBI services in 1993.
Part of the funding challenge, Hinds’ Feet staff said, comes from how difficult it is to classify brain injuries.
“Brain injury is extremely specific,” Rawls said. “In North Carolina, for the behavioral health funding model, it falls under developmental disabilities — but it’s not that. It’s also not mental health, although there’s a lot of overlap with mental health.
“It’s not substance use, although there’s a lot of overlap with that as well — so what is it? It’s a medical diagnosis. It doesn’t really fit into those things.”
In 2022, the state budget allocated $4.9 million to community-based services for people with TBIs, nearly the same amount allocated to the J. Iverson Riddle Developmental Center, one of 14 state-run institutions for people with intellectual and mental disabilities.
North Carolina has long failed to fund home and community-based services at the same level that it funds state institutions. Because of this “institutional bias,” the state was found to be in violation of the landmark 1999 U.S. Supreme Court Olmstead decision, which ruled states must fund services for people with disabilities that enable them to live in the most integrated setting appropriate to their needs.
In addition to being the law, home and community based services — such as those at Hinds’ Feet — are a lot cheaper than institutionalizing people. DHHS’s State Action Plan for People with TBIs, published in 2021, cited a 2015 finding from the Kaiser Family Foundation that found the median cost of home health aide services to be under $46,000 per year, while the median cost of keeping one person in a nursing facility sits at $91,250 annually.
The funding challenges have taught Hinds’ Feet to be nimble, so in order to survive, it must rely on a variety of money pots. The organization gets some funding from Vaya Health — the local mental health managed care organization — in addition to Medicaid waiver programs and county governments. Participants pay to come to Hinds’ Feet, but the directors aim to make the program as accessible as possible. Some use Medicaid, others receive workers compensation or insurance settlements from their injuries, and a handful pay out of pocket — there’s a sliding scale fee that starts at $2 per day.
Being in the community
While Liz shows some of the members how to make biscuits and gravy, others play Uno. As Draw Four, Reverse and some non-confrontational cards pile up on the center deck, the conversation flows from how members got their injuries (car accidents, oxygen deprivation at birth) to how they get to the program each day (some drive, others take the bus; one woman who lives in Yancey County gets picked up by a county transportation service), to how they spent their days before coming to Hinds’ Feet (work, classes at community college).
The work conversation can bring up traumatic memories. Many people with traumatic brain injuries have stories about cruel co-workers, people who mocked their behaviors or made fun of how they spoke.
Before the pandemic, a large part of Hinds’ Feet’s programming was going out in public and doing different activities. It served a dual purpose: for the members to “learn how to be in the community with their new skills,” said day program coordinator Janet Guptill. The activities also gave members of the community opportunities to learn how to interact compassionately with people who have brain injuries.

“How many people [with brain injuries] are sitting in their house watching TV because they can’t get out? [Because] if they do go out, people are going to be like, ‘Why are you acting so strange?’” Guptill said.
“With our people, if we’re in the movie theater and they’re going up to buy a snack, I’ll be behind them, I’ll be there, but I’ll wait,” she said. “Sometimes the clerk will realize, ‘Wait a minute,’ and they will slow down and give them the chance, rather than to be like, ‘What’s wrong with you?’”
Even as many people with brain injuries struggle with short-term memory, often their memories from before the accident are completely intact. That means they know when people are treating them worse than they did in the “before” time.
“That experience of having lived 30 years as a non-disabled person, and then having a situation happen that causes you to now be in this other place is a very unique experience of those with brain injuries, compared with other people with disabilities,” Rawls said.
When limited understanding turns threatening
Even beyond the emotional trauma, the public’s lack of understanding of brain injuries can put people in physical danger. One participant, Devon, knows that first hand.
When he was 19, Devon was walking down his street when a police officer stopped him.

“I was wearing a hoodie, and he thought that I was looking suspicious,” Devon said. The officer told Devon there was an assault nearby, and asked if he knew anything about it. “I was like, ‘No.’ [The officer said], ‘Well, I’m gonna have to talk to your mother and father about that.’ I was like, ‘Okay, but I already told you that I didn’t do anything.’”
Devon said the officer followed him home and put him in handcuffs. “I didn’t know what was going on, so I flipped out,” he remembered. “My mom was crying and my dad was getting upset.”
Devon has lived with a brain injury his whole life. He was born with his umbilical cord wrapped around his neck, cutting off his oxygen supply for a critical amount of time. Later, as an adult, he fell off a ladder at work, which added another injury. He thinks it’s important that everyone learn more about people with brain injuries and how to interact with them, especially police. His intuition is supported by data: studies estimate that half of all people killed by police had a disability.
“We’re normal,” he said. “But we might be walking down the street and a cop pull up and say ‘What are you doing out here?’ And we’ll be shutting down, because we don’t know what to do, what to say.”
When the pandemic recedes, the staff and members hope to restart community activities as soon as possible. If they don’t lead the integration, it’s unlikely anyone else will.
North Carolina Health News is an independent, non-partisan, not-for-profit, statewide news organization dedicated to covering all things health care in North Carolina. Visit NCHN at NorthCarolinaHealthNews.org.![]()



Before you comment
The comments section is here to provide a platform for civil dialogue on the issues we face together as a local community. Xpress is committed to offering this platform for all voices, but when the tone of the discussion gets nasty or strays off topic, we believe many people choose not to participate. Xpress editors are determined to moderate comments to ensure a constructive interchange is maintained. All comments judged not to be in keeping with the spirit of civil discourse will be removed and repeat violators will be banned. See here for our terms of service. Thank you for being part of this effort to promote respectful discussion.